The Retroconversion of Immature Mediastinal Teratoma with Chemothearpy: A Case Report
Mohammad Serajus Salekin and Mohammad Tajul Islam
DOI10.21767/2577-0578.10039
Mohammad Serajus Salekin* and Mohammad Tajul Islam
Department of Cardiovascular and Thoracic Surgery, Dhaka Medical College Hospital, Dhaka, Bangladesh
- *Corresponding Author:
- Mohammad Serajus Salekin
Department of Cardiovascular and Thoracic Surgery
Dhaka Medical College Hospital, Dhaka, Bangladesh.
Tel: +8801973426804
E-mail: drsalekin@gmail.com
Received date: April 10, 2017; Accepted date: May 16, 2017; Published date: May 24, 2017
Citation: Salekin MS, Islam MT. The Retroconversion of Immature Mediastinal Teratoma with Chemothearpy: A Case Report. Insights Chest Dis. 2017, 2:2.
Copyright: © 2017 Salekin MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Mediastinum is a common localization of extra gonadal teratoma. Mediastinal teratoma, which is comprising of 1-5% of all mediastinal tumors is an infrequent germ cell tumor. Immature mediastinal teratoma is a rare malignant neoplasm, which has an abilty to metastasize and recure and histologically resemble embryonal structures. There are few reports in literature, which show post chemotherapeutic retroconversion of immature teratoma; however, retroconversion of mediastinal teratoma into mature teratoma is not common. A 19-year-old boy was diagnosed a case of immature mediastinal teratoma by Computed tomography-guided FNA (Fine Needle Aspiration) and received 6 cycles chemotherapy by bleomycin, etoposide, and cisplatin regimen. After that, surgically total excision of tumor was done and histopathological report reveals mature teratoma, which is presented in this paper.
Keywords
Mediastinum teratoma; Germ cell tumor; Histopathology; Intralesional calcification; Malignant neoplasm; Alpha-fetoprotein; Immature mediastinal teratoma
Introduction
Mediastinal germ cell tumor are rare and represent approximately 1-3% of all germ cell neoplasm [1]. Mediastinal teratoma originates from pluripotent embryonic cells and it differenciates into tissues with all germ cell layers [2]. Mediatinal teratoma is classified into mature, immature, and teratoma with malignant transformation [3]. Most common mediastinal teratoma is benign mature teratoma, which have well differentiated germinal tissues, mainly comprising of ectodermal tissues. Immature teratoma has immature germinal derivatives. Immature mediastinal teratoma are rare, found in only 1% of all mediastinal teratoma [4]. About 36% of patients with mediastinal tumor are asymptomatic at the moment of diagnosis [5]. When symptoms are present, they may be due to compression, invasion of intrathoracic structures or diagnosed by chance during chest imaging. Computed Tomography (CT) of chest is the first investigation of choice to confirm the diagnosis and to indentify the extent of mediastinal tumor. Mediastinal benign teratoma is usually well circumscribed and it gives radiographic features of multilocular cystic, solid, and fatty components with calcification. However, these radiographic features is not present in all cases and only 20-40% of cases give features of calcifications [2,6]. On the other hand, on CT mediastinal immature teratoma manifests as a heterogenous mediastinal mass containing soft tissue fluid, fat, calcification, or any combination of four [7]. Increasing value of tumor markers like alpha-fetoprotein and human chorionic gonadotropin hormone may suggest malignancy. Treatment of immature teratoma in surgery and chemotherapy [8]. Retroconversion of immature malignant tumor by chemotherapy where chemotherapeutic eliminates malignant component of tumor or altered tumor cell structure, which transforming totipotent malignant germ cell into mature benign teratoma. A case in which the patient was received chemotherapy due to immature medistinal mass diagnosed by CT guided FNA and mature mediastinal teratoma is detected through the biopsy is conducted after the total surgical excision of tumor, subsequently is presented in this paper.
Case Report
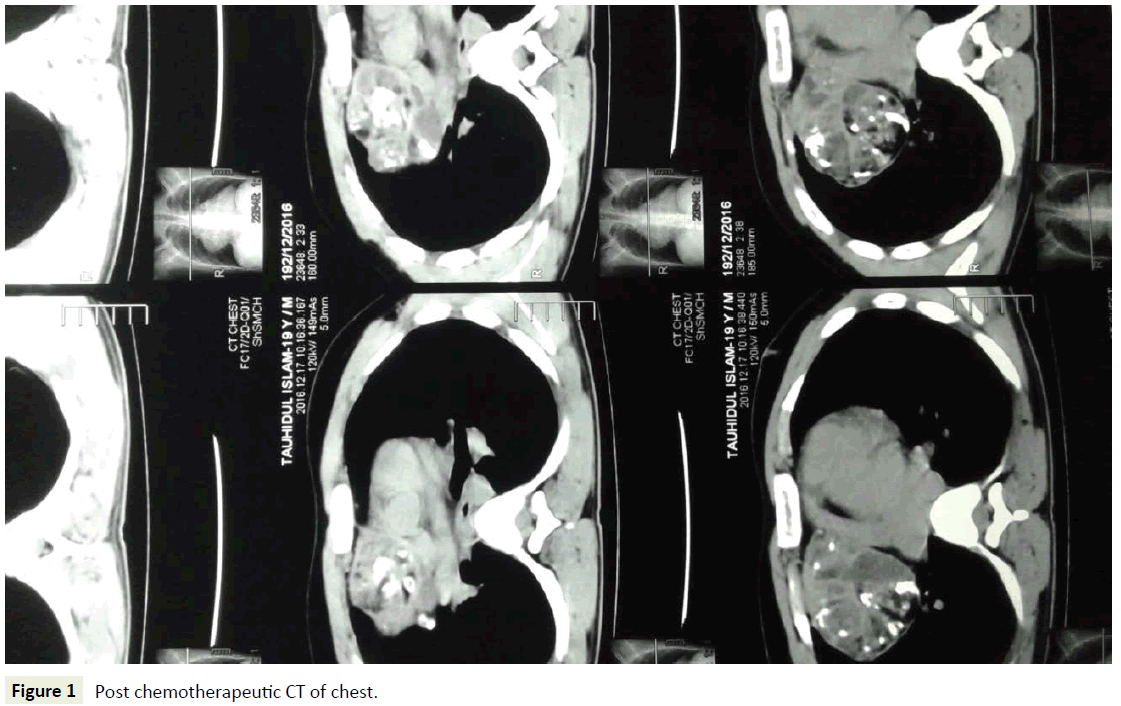
A 19-year-old boy presented with occasional fever, productive cough, chest pain, and weight loss for last six months, which is for 1-1½ months interval present 3-4 days is resolved by antibiotics and analgesics. On x-ray chest Posterior Anterior view, a large well marginated mass on anterior mediastinum extending to the right hemithorax with obliteration of both cardiophrenic and costophrenoc angles. On CT chest, one large irregular slightly enhancing soft tissue density mass lesion having intralesional calcification is noted in the right anterior mediastinum, measuring about 13 × 10 cm in size and mediastinum shifted to the left and encysted pleural effusion in the right pleural cavity. Tube thoracostomy was done for severe respiratory distress about 1200 ml haemorrhagic fluid came out and subsequent days chest drain tube collection gradually decreased, chest drain tube is removed on 7th postoperative day. Tumor markers Alpha- Fetoprotein (AFP) 30954 ng/ml, Human Chorionic Gonadotropin (hCG) 0.25 mIU/ml, Lactatedehydrogenase (LDH) 358 U/L. Fineneedle aspiration (FNA) from mediastinal mass positive for malignant teratoma. He has received 6 cycles chemotherapy bleomycin, etoposide, cisplatin regimen, where first four cycles by Inj. Bleomycin 30 mg (Day 1,8,15), Inj. etoposide 150 mg (Day 1-5), Inj. cisplatin 30 mg (Day 1-5), fifth cycle by Inj. etoposide 150 mg (Day 1-5), Inj. cisplatin 30 mg (Day 1-5) and sixth cycle by tab. etoposide 50 mg twice daily for 5 days. After receiving 1st cycle chemotherapy, his tumor markers are reduced alphafetoprotein 54.16 ng/ml, hCG <1.2 mIU/ml and reduce size of mediastinal mass. After completion of 6 cycles chemotherapy, he was evaluated by clinically, measuring tumor markers and radiologically by Chest x-ray and CT scan of chest with contrast. Tumor markers AFP 3.57 ng/ml, LDH 214 U/L, hCG <1.20 IU/L. Chest x-ray shows dense homogenous opacity in mid and lower zones of right lung field, which was not separated from the mediastinum, scattered calcification in lower zone of lesion (Figure 1).
Figure 1: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
CT chest finding is well defined capsulated mixed density large mass measuring about 8 × 7.5 cm having areas of fat density, scattered calcifications and dental element is noted in anterior and middle mediastinum on right side. Superior venacava is compressed by mass but fat plane is maintained. Per operative findings is huge mass about 7 × 7 cm in size adhere with lung, pericardium present in middle mediastinum in between heart and lung and cut section shows areas of fatty tissue, cartilage, hair follicles, bone tissues. After total excision of mediastinal mass histopathology report reveals mature teratoma and post operatively tumor markers alpha feto protein 2.74 ng/ml and HCG 1.13 mIU/ml (Figure 2).
Figure 2: HPLC chromatogram of the nine reference compounds in 50% aqueous methanol, measured at 370nm. Retention times for rutin, sutherlandin A, sutherlandin B, kaempferol-3-O-rutinoside, sutherlandin C, sutherlandin D, quercitrin, quercetin and kaempferol were 11.9, 12.7, 13.8, 15.3, 16.2, 17.0, 18.0, 26.2 and 28.1 minutes, respectively.
Discussion and Conclusion
In contrast to ovarian and sacrococcygeal region, the mediastinum is a rare location for a teratoma, Schneider et al. describes two German studies where 1193 patients were diagnosed with testicular and nontesticular germ cell tumor and only 4.3% of these patients had a mediastinal teratoma [9]. The most common location of extra gonadal germ cell tumor is anterior mediastinum [10,11]. Mediastinal germ cell tumor represent approximately 15% of anterior mediastinal tumor in adult and 24% in children. Benign germ cell tumors occur in male and female patients with equal frequency. However, male patients suffer from germ cell tumor most commonly. Mature teratoma followed by Seminoma is the most common histologic type of mediastinal germ cell tumor [1]. Germ cell tumor commonly affect patients below age of 30 years and in childhood. Only 3% and 20% of all teratoma is immature teratomaand malignant teratoma respectively. Immature teratoma differs from benign teratomas in terms of tissue component that observed in fetus or embryo. Any type of tissue may be found in immature teratoma, most common is neurogenic. Immature teratoma grow rapidly and metastasized by penetrating the capsule. The most distinctive feature distinguishing malignant teratoma from mature teratoma is the neuroectodermal components that involves. The pathogenesis of extragonadal immature teratoma is not understood completely yet. However clinically, it is impossible to differentiate mature teratoma from immature teratoma. It can be differentiated only by careful histological examination. Determination of serum tumor markers Alpha Fetoprotein (AFP) and HCG is important in the diagnosis and follow up of mediastinal germ cell tumors. Differently from immature teratomas, patient with benign teratomas have normal tumor markers [12-15]. CT of chest is the first choice for the diagnostic evaluation of immature and mature mediastinal teratoma. It shows tumor location and extention as well as intrinsic elements including soft tissue, fat, fluid and calcification [16]. The mediastinal immature teratoma menifests as a heterogenous mediastinal mass containing soft tissue fluid, fat or calcification or any combination of four. Mediastinal mature teratomas typically manifest on CT chest as a heterogenous sharply marginated spherical or lobulated mediastinal masses containing soft tissue, fat, fluid and calcium attenuation or any combination of the four. Fat fluid levels, considers highly specific for the diagnosis of the mediastinal mature teratoma, which are uncommon [7]. The mediastinal masses can give differential diagnosis like mediastinal fat pad, mediastinal lipomatosis, lipoma, omental herniation, thymolipoma and liposarcoma. However, immature teratoma due to their cystic appearance with predominance of fluid elements and high frequency of calcification, findings readily seen on CT scans which can be easily differed from these lesions.
In our case, after chemotherapy CT Chest shows a heterogenous smooth-lobuleted edged mass which arises from the right anterior mediastinum comprising of soft tissue, fluid, fat and calcification.
In 15 years aged patients with immature mediastinal teratoma, complete surgical resection is absolutely necessary. Long survival can be expected after complete resection combined with chemotherapy [4]. Mature tissues might co-exist with immature tissues in many germ cell tumors. Theoretically it is expected that chemotherapy will eliminate the malignant component but may lead to the growth of the benign component. After that only benign mature elements left behind; tumor cell structures being altered by chemotherapy and totipotent malignant germ cell transforms into mature benign teratoma [17]. Another theory for Growing Teratoma Syndrome (GTS) is “Chemotherapeutic Recoversion” of the immature teratoma cells into mature teratoma [8]. In chemotherapeutic retroconversion of immature malignant tumor, normalization of an initially raised serum tumor marker and CT features of maturation which include increased density of mass lesions, margins become better circumscribed in relation to adjacent tissues and the onset of internal calcification, with fatty areas and cystic changes [18].
Conclusion
Immature mediastinal teratoma is a rare tumor and it is different from benign teratoma. This differentiation can only be made by histological examination. CT of chest is the radiological examination tool for the diagnostic evaluation of mediastinal teratoma with tumor markers alpha fetoprotein, HCG. Combined chemotherapy with total surgical excision of tumor treatment of choice. Chemotherapeutic retroconversion is uncommon in teratoma. Confirmation by biopsy should be done for confirming the occurrence of new tumors in the follow up of patients with germ cell tumors.
Acknowledgement
Department of Radiology and Imaging, Pathology and Oncology of Dhaka Medical College Hospital, Dhaka, Bangladesh.
Financial Disclosure
The authors declared that this study has received no financial support.
Conflicts of Interest
No conflicts of interest to disclose was declared by authors with others: 1) Registrar, Thoracic Surgery, DMCH. 2) Medical officer, Cardiac Surgery, DMCH.
References
- Nichols CR (1991) Mediastinal germ cell tumors: Clinical features and biologic correlates. Chest 99: 472-479.
- De Hoyos A, Sundaresan RS (2001) Resection of mediastinal Teratoma. Oper Tech Thorac Cardiovasc Surg 6: 209-220.
- Jothianandan K, Tibb AS, McLemore M, Keller S, Appel DW (2010) An adult man presenting with hemoptysis caused by mature teratoma with rupture into the bronchus and pericardium and complicated by Haemophilus influenzae infection. J Thorac Cardiovasc Surg 139: e104-e107.
- Das BB, Richardson C, Lala R, Sahoo S (2001) Primary immature Mediastinal teratoma in a Newborn. Indian Pediatr 38: 1181-1184.
- Lewis BD, Hurt RD, Payne WS, Farrow GM, Knapp RH, et al. (1983) Benign teratomas of the mediastinum. J Thorac Cardiovasc Surg 86: 727-731.
- Santos PC, Maia CP, Pereira JC, Oliveira TC (2007) Giant mediastinal teratoma found during surgery after thoracic teratoma. Rev Bras Cir Cardiovasc 22: 252-254.
- Choi SJ, Lee JS, Song KS, Lim TH (1998) Mediastinal teratoma: CT differentiation of ruptured and unruptured tumors. AJR Am J Roentgenol 171: 591-594.
- DiSaia PJ, Saltz A, Kagan AR, Morrow CP (1977) Chemotherapeutic retroconvertion of immature teratoma of the ovary. Obstet Gynecol 49: 346-350.
- Schneider DT, Calaminus G, Koch S, Teske C, Schmidt P, et al. (2004) Epidemiologic analysis of 1,442 children and adolescents registered in the Germam germ cell tumor protocols. Pediatr Blood Cancer 42: 169-175.
- Rosai J, Levine GD (1976) Tumors of the thymus. Atlas of Tumor Pathology. Second series, Fascicle 13, Washington, D.C., Armed Forces Institute of Pathology pp: 1-21.
- Marchevsky AM, Kaneko M (1984) Surgical pathology of the mediastinum. Raven Press, NY, USA.
- Ulbrigth TM (2005) Germ cell tumors of gonads: A selective review emphasizing problems in differential diagnosis, newly appreciated and controversial issues. Mod Pathol 18: 561-579.
- Col C (2003) Immature teratoma in both mediastinum and liver of a 21-year-old female patient. Acta Med Austriaca 30: 26-28.
- Hiroshima K, Toyozaki T, Iyoda A, Yusa T, Fujisawa T, et al. (2001) Apoptosis and proliferative activity in mature and immature teratomas of the mediastinum. Cancer 92: 1798-1806.
- Taniyama K, Ohta S, Suzuki H, Matsumoto M, Nagashima Y, et al. (1992) Alpha-fetoprotein-producing immature mediastinal teratoma showing rapid and massive recurrent growth in an adult. Acta Pathol Jpn 42: 911-915.
- Drevelegas A, Palladas P, Scordalaki A (2001) Mediastinal germ cell tumors: a radiologic–pathologic review. Eur Radial 11: 1925.
- Hong WK, Wittes RE, Hajdu ST, Cvitkovic E, Whitmore WF, et al. (1977) The evolution of mature teratoma from malignant testicular tumors. Cancer 40: 2987-2992.
- Moskovic E, Jobling T, Fisher C, Wiltshaw E, Parsons C (1991) Retroconversion of immature teratoma of the ovary: CT appearances. Clin Radiol 43: 402-408.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences