Preference for Smaller Diameter Mouthpiece in Performing Dynamic Lung Function Tests: A Consideration for Patients
Anjanna Kukreja, Alyson Su-Yin Tan, Strachan Zhi-Hui Teoh and Li-Cher Loh
DOI10.21767/2577-0578.10012
PMC Lung Research, Department of Medicine, Penang Medical College, Malaysia
- *Corresponding Author:
- Li-Cher Loh
Department of Medicine, Penang Medical College
4 Jalan Sepoy Lines, Georgetown, 10450 Penang
Malaysia
Tel: +6042287171
Fax: +6042284285
E-mail: richard_loh@pmc.edu.my
Received date: December 14, 2015; Accepted date: February 10, 2016; Published date: February 18, 2016
Citation: Kukreja A, Su-Yin Tan A, Teoh SZH. Preference for Smaller Diameter Mouthpiece in Performing Dynamic Lung Function Tests: A Consideration for Patients.Insights Chest Dis. 2016, 1:12.
Short Commentary
Many have suspected that mouthpiece with a smaller diameter is easier to make a forced expiration in spirometry or peak flow meter. This may be related to the ease of making a tight lip seal over a smaller opening than a larger one while operating the maneuver of a forced expiration. Those who are breathless or having diseased lung may struggle more over this. Some may prefer a smaller mouthpiece to conduct this maneuver because of the same reason. To our knowledge, this aspect of personal preference has not been studied before.
In a prospective cross-sectional study, we compared the individual preferences of mouthpiece size when conducting either spirometry (MicroLab™ spirometer) in 51 young adults (mean (SD) age 23 (1.5) years) or peak flow meter measurement in 50 older adults [age 59 (10.6) years]. Both groups were gendermatched (overall 47% male) and recruited among from a medical college and a large urban-based teaching hospital. Subjects with any acute or chronic lung diseases were excluded. The bigger mouthpiece studied was the commonly available single-use cardboard disposable mouthpiece (30 mm diameter) [Micro Medical Adult Disposable Mouthpiece; code: MMPSA 1000] and the smaller one studied was a reusable 22 mm-diameter mouthpiece [Micro Medical Universal Mouthpiece (code: MMPSA 2200)]. The issue of interest here was about the mouthpiece size. Verbal consent was obtained from all subjects. This study was performed as part of a larger COPD study approved by the local research and ethics committee.
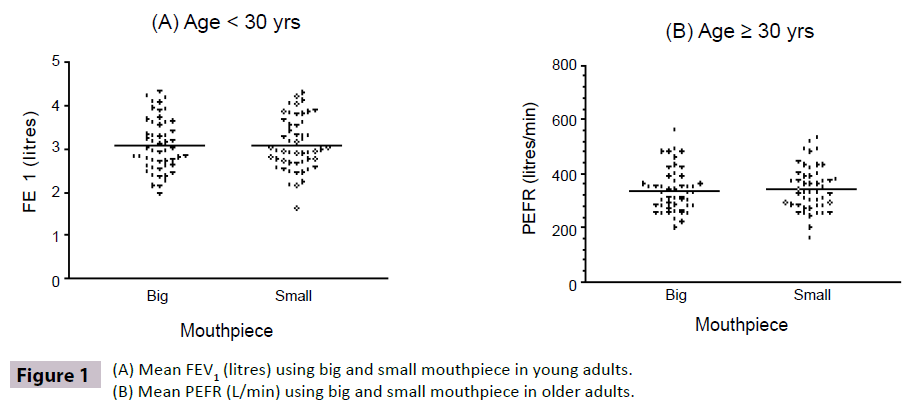
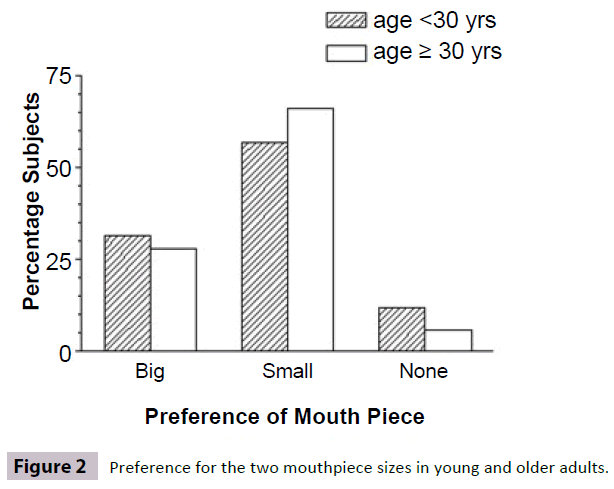
Mean Forced Expiratory Volume in One Second (FEV1) was not statistically different when either big or small mouthpiece was used [Mean (SD) 3.06 (0.083) vs. 3.08 (0.083) litres; p = 0.32, paired t-test] in young adults (Figure 1A). Mean Peak Expiratory Flow Rate (PEFR) [1] was also not statistically different when either big or small mouthpiece was used [Mean (SD) 336 (11.4) vs. 343 (11.8); p = 0.16] in older adults (Figure 1B). The number of subjects who preferred the smaller mouthpiece was about twice the number who preferred the bigger one [young adults, 29 (56.8%) vs. 16 (31.3%); older adults, 33 (66%) vs. 14 (28%)].
Six (11.7%) young and three (6%) older adults did not have a preference (Figure 2).
Our study showed that mouthpiece size does not affect the consistency of measurement in either spirometry or peak flow meter in healthy adults. This is not surprising as mouthpiece diameter size of 30 mm and 22 mm are well attested in science and experience to be used for channeling unimpeded flow in lung function tests. Mouthpiece with size smaller than 22 mm like the spirettes used in EasyOne® Plus spirometry has also been long used in international multi-center studies like Burden of Obstructive Lung Disease (BOLD) [2] and presents no measurement problems. Our study however showed a clear preference for smaller size mouthpiece compared to the standard 30 mm one that is commonly used. We assume that this is due to the ease of making a tight lip seal over the mouthpiece with smaller ones. While this is observed in healthy subjects without lung conditions, it is possible that subjects who are breathless or with chronic lung diseases may also have such preference since making such maneuver can be even more difficult.
Dynamic lung function tests like spirometry and PEFR measurement is highly effort-dependent on part of the subject. Maximal airflow occurs during this effort-dependent portion of the inspiratory and expiratory maneuver. As such, low values may be caused by a less-than-maximal effort of the subject than by genuine airflow obstruction or diseased lung. A preferred mouthpiece to optimize lip seal and these dynamic breathing maneuvers may optimize this effort-dependent measurement. Our findings suggest that a smaller mouthpiece should be available more widely for patients since it appears to be a preferred option. This may improve adherence especially if subjects are asked to conduct such tests by themselves like in the case of home PEFR measurement in selfmanagement of asthma [3].
Acknowledgement
The authors acknowledged with thanks the support from the Penang Medical College Student Council and Hospital Director of Penang Hospital for this study.
References
- Miller MR, Dickinson SA, Hitchings DJ (1992) The accuracy of portable peak flow meters. Thorax 47: 904-909
- Buist AS, Vollmer WM, Sullivan SD, Weiss KB, Lee TA (2005) The Burden of Obstructive Lung Disease Initiative (BOLD): rationale and design. COPD 2: 277-283.
- Partridge MR(1994) Asthma: guided self-management. BMJ 308: 547-548
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences