Pleural Effusions
Funda Ozturk Incekara*, Deniz Kaygusuz Tikici and Hakan Nomenoglu
DOI10.21767/2577-0578.10040
Funda Ozturk Incekara*, Deniz Kaygusuz Tikici and Hakan Nomenoglu
Department of Thoracic Surgery, Ataturk Chest Diseases and Thoracic Surgery Trained and Research Hospital, Ankara, Turkey
- *Corresponding Author:
- Funda Ozturk Incekara
Department of Thoracic Surgery
Ataturk Chest Diseases and Thoracic Surgery Trained and Research Hospital
Ankara, Turkey
Tel: 00905057682387
E-mail: drfundaincekara@gmail.com
Received Date: January 15, 2018; Accepted Date: January 22, 2018; Published Date: February 05, 2018
Citation: Incekara FO, Tikici DK, Nomenoglu H (2018) Pleural Effusions. Insights Chest Dis 3:1.
Abstract
Introduction
Pleural effusion is defined as a fluid collection between the pleural leaves due to local/systemic disease of the pleura, lung or extrapulmonary organs. Normally, 0.1 to 0.2 ml/kg of fluid is present in the pleural leaves to facilitate pleural movement. When the balance between the production and reabsorption of this fluid deteriorates, it becomes pleural effusion [1].
Mechanisms of pleural effusion can be summarized as [1,2].
• Increased hydrostatic pressure in the microvascular circulation
• Decreased oncotic pressure in the microvascular circulation
• Increased negative pressure in the pleural space
• Separation of pleural leaves
• Increased permeability in the microvascular circulation
• Decrease in lymphatic drainage capacity
• Transition from the abdomen to the thorax
The prevalence of pleural effusion is estimated at 320/100000 and is seen as equal in both genders. However, malignant effusions are more common in women due to breast and gynecological cancers, while malignant mesothelioma and pancreatitisassociated effusions are more frequent in males [3].
Causes of Pleural Effusion
Transudative pleural effusions
•Congestive heart failure
•Cirrhosis
•Nephrotic syndrome
•Kidney failure
•Peritoneal dialysis
•Urinothorax
•Myxoedema
•Hypoalbuminemia
•Atelectasis
•Sarcoidosis
•Pulmonary embolism
•Vena cava superior syndrome
•Meigs syndrome
•Constrictive pericarditis
•Cerebrospinal fluid leakage to pleural space
Exudative pleural effusion
•Neoplastic diseases
•Metastatic diseases
•Mesothelioma
•Lymphoma
•Infectious diseases
•Bacterial infections
•Tuberculosis
•Fungal infections
•Parasitic infections
•Viral infections
•Pulmonary embolism
•Cardiovascular diseases
•Coronary artery bypass surgery
•Postcardiac injury syndrome
•Pericardial diseases
•Gastrointestinal diseases
•Pancreatic diseases
•Subphrenic, intrahepatic, intrasplenic abscess
•Esophageal perforation
•Abdominal surgery
•Diaphragm hernia
•Liver transplantation
•Collagen vascular diseases
•Rheumatoid pleurisy
•Systemic lupus erythematosus
•Drug induced lupus
•Immunoblastic lymphadenopathy
•Sjögren's syndrome
•Familial Mediterranean fever
•Churg-Strauss syndrome
•Wegener granulomatosis
•Gynecology and Obstetrics
•Ovarian hyperstimulation syndrome
•Fetal pleural effusion
•Postpartum pleural effusion
•Meigs syndrome
•Endometriosis
•Diseases of lymphatic system
•Chylothorax
•Yellow nail syndrome
•Lymphangioleiomyomatosis
•Drug induced
•Nitrofurantoin
•Dantrolene
•Methylsergide
•Ergot alkaloids
•Amiodarone
•Interleukin-2
•Procarbazine
•Methotrexate
•Clozapine
•Mitomycin
•Bleomycin
•Bromocriptine
Other
•Asbestos exposure
•Lung transplantation
•Bone marrow transplantation
•Trapped lung
•Radiation exposure
•Drowning
•Amyloidosis
•Thoracotomy
•Electrical burns
•Extramedullary hematopoiesis
•ARDS
•Syphilis
•Iatrogenic pleural effusions
•Haemothorax
•Idiopathic pleural effusions
Diagnostic Approach in Pleural Effusion
1. Clinic presentation: Patient's history and physical examination
2. Radiology: Conventional radiography, ultrasonography, computerized tomography
3. Thoracentesis: pleural fluid analysis
4. Bronchoscopy
5. Pleural fine needle biopsy
6. Video assisted thoracoscopic surgery (VATS) - Tauroctony (open pleural biopsy)
Clinical approach
Pleural effusion disturbs the patient's respiratory mechanics and leads to restrictive type of respiratory failure. Total lung capacity, functional capacity and forced vital capacity decrease. Ventilation/perfusion imbalance and/or ventricular diastolic collapse may occur depending on the amount of atelectasis caused by effusion. Therefore, the most common symptom is dyspnea and mild, nonproductive cough. Depending on the underlying disease, night sweats, weight loss, hemoptysis and high fever can also be seen.
Physical examination findings may vary depending on the amount of effusion. It is clinically nonexistent until reaching a volume of 300 ml. However, when this amount is exceeded; less participation to the respiration of the hemithorax, matty in the percussion examination, decreased vocal fremitus, decrease or absence of breath sounds, pleural rub may occur. Mediastinal shift may occur when the pleural effusion reaches 1000 ml. This results in a physical examination of the trachea as a counter-deviation to the opposite side. Depending on the underlying disease, peripheral edema, swelled neck veins, S3 rhythm, cutaneous findings or lymphadenopathies may be detected [4-7].
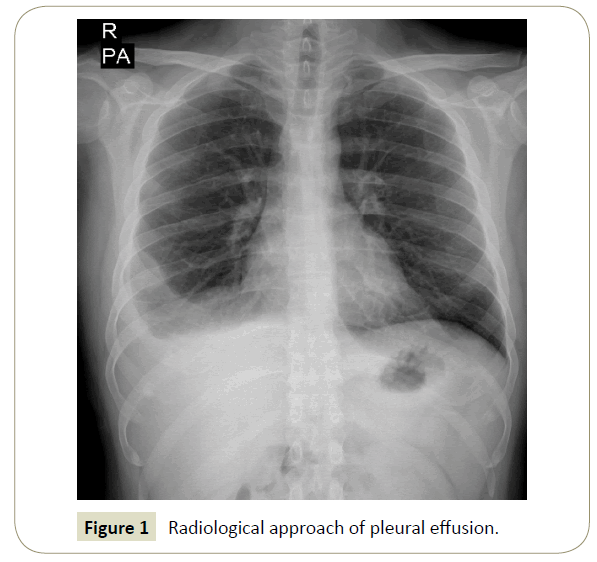
Radiological approach
The first procedure to be performed in a patient with suspicion of pleural effusion on physical examination is to evaluate the patient with radiological examinations. Approximately 50 ml of fluid can be seen on the lateral chest radiograph and 200 ml of fluid can be seen on posterior-anterior chest radiograph. However, in radiographs taken in a supine position, the fluid does not cause significant blunting of the sinuses while it spreads to the entire thorax (Figure 1).
Ultrasound can reveal important findings in cases where effusion is suspected. It helps to distinguish solid structures, to locate locular or small amount of pleural effusion or to perform thoracentesis safely.
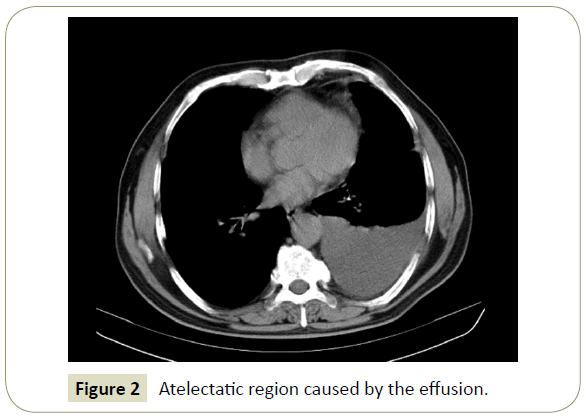
Computed thorax tomography is useful in the complicated cases or situations where anatomy cannot be clearly demonstrated. However, it is more appropriate to see the pathology after the fluid has been emptied in order to reveal pathologies that may be in the atelectatic region where caused by the effusion (Figure 2) [6,7].
Thoracentesis
The easiest way to sample the pleural effusion is thoracentesis. Thoracentesis allows us to know if the fluid is transudate or exudate. This discrimination is made with the Light criteria. Transudative fluids are low in protein content and develop as a result of imbalance between hydrostatic and oncotic forces that affect the pleural fluid cycle or as a result of lymphatic obstruction. Exudative fluids may occur due to increased permeability on the pleural surface and microvascular structures, and protein content is high. Discrimination of transudate/exudate is important for differential diagnosis and for the determination of treatment afterwards (Table 1) [1,2].
| Pleural fluid protein/serum protein | >0.5 | Exudate |
| Pleural fluid LDH/serum LDH | >0.6 | |
| Pleural fluid LDH | >2/3 of normal serum LDH |
Table 1: Light criteria.
Pleural fluid biochemistry and blood biochemistry have to be studied together and simultaneously for the evaluation of the Light criteria. However, differentiation can be made by evaluating only pleural fluid biochemistry. The cholesterol level of the pleural fluid is 45 mg/dl and the pleural fluid protein value is over 2.9 g/ dl, which alone is sufficient for exudate diagnosis [4].
The studies suggested to determine the etiology of pleural fluid are as follows:
1. Macroscopic appearance of the fluid
2. Cell counting and differentiation in the pleural fluid
3. Pleural fluid smear and cultures
4. Pleural fluid glucose and LDH measurement
5. Cytologic evaluation of the pleural fluid
6. Examination for tuberculosis
Pleural fluid smear and cultures: Gram staining, bacteria, mycobacteria and fungus cultures should be performed routinely. Positivity may increase if planting directly to the medium just beside the patient [3,4] (Table 2).
| Color, turbidity, viscosity, odor | Diagnosis |
|---|---|
| Light yellow color, clear | Transudatice effusion |
| Straw yellow, fibrin nets | Tuberculosis |
| Viscous, burgundy red | Malignant Pleural Mesothelioma |
| In the appearance of chocolate sauce | Amoeba abscess |
| Black | Aspergillosis |
| Yellowish-green | Rheumatoid pleurisy |
| Hemorrhagic | Trauma, malignancy |
| White | Chylothorax, pseudochylothorax, empyema |
| Pus | Empyema |
| Food particles | Esophageal rupture |
| Turbid appearence | Increased cellular ingredients, lipids |
| Putrid smell | Anaerobic infections |
| Urine smell | Urinothorax |
Table 2: Diagnostic approach according to appearance of pleural fluid.
Cytologic examination of pleural fluid: If malignancy is suspected, pleural fluid cytology is a rapid, effective and noninvasive diagnostic method. Diagnosis positivity varies between 40-87%. Experience of the pathologist, increased tumor burden, tumor growth in the pleural space, and 3 times repetition of cytology may increase the positivity [3,4].
Examination in terms of tuberculosis: It is possible to diagnose tuberculosis by polymerase chain reaction (PCR) for adenosine deaminase (ADA), gamma interferon and mycobacterial DNA in the pleural fluid. When the gamma interferon level is above 5 U/ ml, diagnose can be differentiated by nearly 100% of sensitivity and specificity. In addition, pleural fluid/serum gamma interferon ratio> 20 leads to differential diagnosis (Tables 3 and 4) [3,4].
| Erythrocyte | Hemorrhagic pleural effusion: > 5.000 / mm3 erythrocytes, pleural fluid Hct >1% Hemothorax: > 100,000 / mm3 erythrocytes, pleural fluid/blood Hct >0.5 • Trauma • Lung cancer • Mesothelioma • Pulmonary embolism • Tuberculosis • Coxsackie virus infection • Postcardiac injury syndrome (PCIS) • Asbestosis • Hemorrhagic pancreatitis |
| Neutrophils | Acute inflammation indicator • Pneumonia • Empyema • Pulmonary embolism • Lung abscess • Subphrenic abscess • Tuberculosis (Early period) • Pancreatitis • 10% of transudative fluids |
| Lymphocytes | Lymphocytosis: 85-90% lymphocytes in the pleural fluid • Tuberculosis • Malignant pleural effusion • Lenfoma • Sarcoidosis • Rheumatoid pleurisy • Fungal diseases |
| Eosinophils | Eosinophilia: >10% eosinophil in pleural fluid The most common cause is thoracentesis-induced air and blood • Hemothorax • Pneumothorax • Lung infarction • Parasitic diseases (hydatid cyst, amebiasis, ascariasis, paragonimiasis) • Fungal diseases (Histoplasmosis, coccidioidomycosis) • Drug-induced pleural effusion • Asbestosis • Pulmonary embolism |
| Basophils | Basophilia: >10% basophil in pleural fluid • Leukemic infiltration of the pleura |
| Plasmocyte | In abundance; • Multiple myeloma |
| Mesothelial cell | They are mainly seen in transudates <5% mesothelial cells in pleural fluid; • Tuberculosis • Empyema • Rheumatoid pleurisy • Malignancy • Use of sclerosing agent |
Table 3: Diagnostic approach to pleural fluid according to cell dominance.
| Examination | Diagnosis |
|---|---|
| Pleural fluid glucose <60 mg/dL or Pleural fluid/serum glucose <0.5 |
Empyema Rheumatoid pleurisy Tuberculosis Malignancy Paragonimiasis Haemothorax Esophageal rupture Churg-Strauss' syndrome Urinothorax |
| Conditions detected in pleural fluid pH <7.20 | Complicated parapneumonic effusion Esophageal rupture Rheumatoid pleurisy Tuberculosis Malignancy Systemic acidosis Haemothorax Paragonimiasis Urinothorax |
| The lowest pH level in the pleural fluid | Esophageal rupture |
| Low pH value in transudates | Urinothorax |
| Conditions with pleural fluid LDH >1000 IU/L | Empyema Complicated parapneumonic effusion Rheumatoid pleurisy Paragonimiyazis Collagen tissue diseases |
| ADA (Adenosine deaminase) | >40 IU/L differentiation of tuberculosis and malignancy >70 IU/L Tuberculosis |
| ADA elevation situations | Tuberculosis Rheumatoid pleurisy Empyema Lymphoma Leukemia |
| Pleural fluid / serum amylase >1 | Acute pancreatitis Pancreatic pseudocyst Esophageal rupture Malignancy Ruptured ectopic pregnancy |
| Pleural fluid lysozyme> 20 μg/mL or Pleural fluid / Serum lysozyme >1.2 Pleural fluid cholesterol> 90 mg/dL |
Distinguishes tuberculous pleurisy from malignancy. Tuberculosis possibility increases. |
| Pleural fluid triglyceride> 110 mg/dL | Chylothorax |
| Pleural fluid triglyceride is between 50-110 mg/dL and chylomicrons in lipoprotein analysis |
Chylothorax |
| Pleural fluid triglyceride <50 mg/dL and Pleural fluid cholesterol> 250 mg/dL |
Pseudochylothorax |
| Pleural fluid hyaluronic acid> 1 mg/mL M. | Mesothelioma |
| Pleural fluid / serum creatinine >1 | Urinothorax |
Table 4: Biochemical examinations in pleural fluid diagnostic approach.
Bronchoscopy
Diagnostic application, recommended in case of hemoptysis, atelectasis, parenchymal lesion, central lung lesion or massive pleural effusion [4,5].
Pleural needle biopsy
It is indicated in patients who cannot be diagnosed by less invasive methods. Pleural biopsy; closed pleural biopsy, biopsy under CT or thoracoscopic biopsy. Under CT, pleural biopsy provides reliable results when the pleural thickening is over 1 cm [8,9].
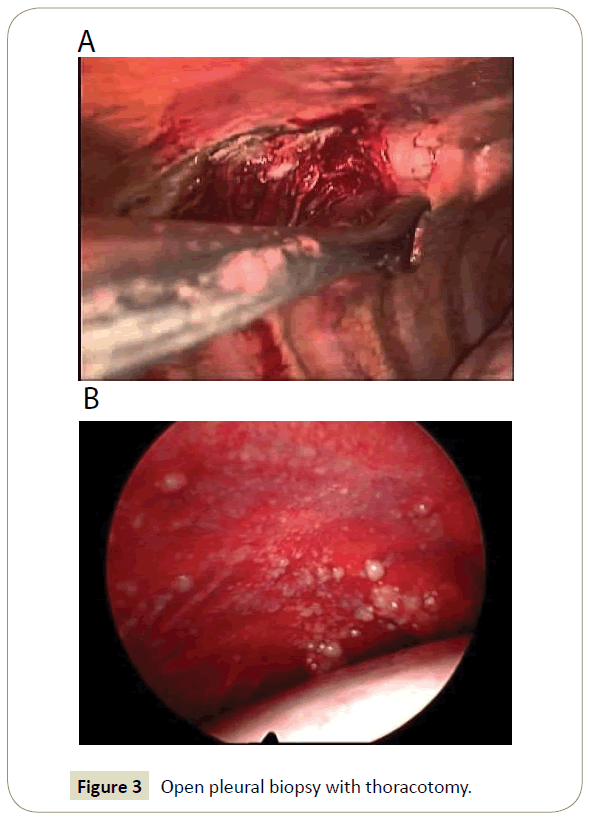
Video assisted thoracoscopic surgery (VATS) - Thoracotomy (Open pleural biopsy)
Pleural biopsy with VATS provides both inspecting pleural surfaces, performing biopsy from the suspicious regions of the pleura and draining the effusion at the same time [5]. It can be done under intubated general anesthesia; also, can be done under non-intubated general anesthesia or paravertebral block/ thoracal epidural anesthesia.
Open pleural biopsy with thoracotomy is a useful choice in cases where pleural leaves are over-thickened and pleural space is absent due to cohesions between pleural leaves as shown (Figure 3A and B).
References
- Rusch VW (2002) Pleural effusion: benign and malignant. In: Thoracic Surgery, 2nd edn. Churchill Livingstone, New York, pp: 1157–1170
- Shields TW (2007) Anatomy of the pleura. In: General thoracic surgery, 7th Edn. Lippincott Williams & Wilkins, Philadelphia, USA, pp: 729-735.
- Yataco JC, Dweik RA (2005) Pleural effusions: Evaluation and management. Cleve Clin J Med 72: 854-872.
- Light RW (2001) Pleural Diseases. 4th Edn. Lippincott Williams & Wilkins, Phialdelphia, USA.
- Light RW (2002) Diagnostic approach in a patient with pleural effusion. Eur Respir Mon 22: 131-145.
- Winterbauer RH (1998) Nonmalignant pleural effusions. In: Fishman AP (Edn). Fishman’s pulmonary diseases and disorders. New York: McGraw-Hill, pp: 1411-1427.
- Zimmerman LH (1997) Pleural effusions. In: Goldstein RH, O’Connell JJ, Karlinsky JB (Eds). A practical approach to pulmonary medicine. Philadelphia: Lippincott-Raven, pp: 195-205.
- Light RW (2002) Pleural effusion. N Eng J Med 346: 1971-1977.
- Light RW (1997) Diagnostic principles in pleural disease. Eur Respir J 10: 476-481.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences